When Fainting Spells Heart Trouble
November 12, 2018
When Corie Cutshall was just 6 years old, she was sent home from school after complaining of feeling lightheaded and dizzy. She experienced the same feeling without explanation while at a friend's house in 4th grade. And in 8th grade, she passed out during a finger-prick blood test, actually falling off the exam stool.
"Since I can remember, I've always passed out pretty easily," Corie says. "I'd seen a few doctors about it and they didn't think it was a big deal. I thought, 'Maybe this is totally normal and I'm just a crazy person.'"
As time went on, Corie's fainting spells became more frequent and severe. She started to experience seizure-like symptoms when she fainted. Most of the time, she felt tired, dizzy and lightheaded, but she brushed off her symptoms.
"I just thought I was dehydrated, so I'd drink more water," Corie explains. "It was one of those situations where you think something might be wrong, but you don't want there to be, so you just kind of ignore it."
That changed on Dec. 2, 2014. After a blood draw, Corie was driving to work in rush hour traffic when she began to feel lightheaded and sick. Knowing these symptoms usually preceded a fainting spell, she tried to pull over but couldn't get off the road in time. Corie fainted at the wheel and her car veered off the freeway and into an embankment. Luckily, no one was hurt and Corie made it out with only minor injuries.
"That's when I decided I needed to get serious."
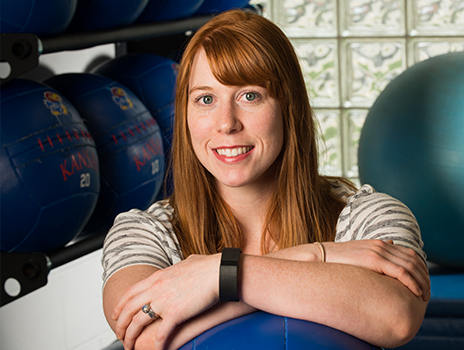
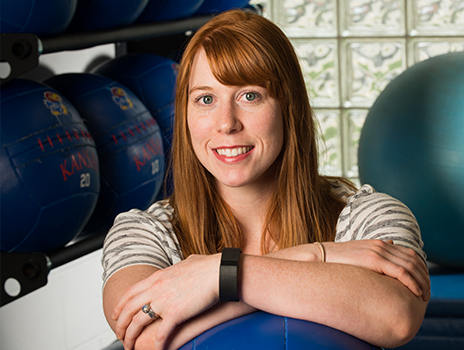
After her accident, Corie decided to make an appointment with a cardiologist. She had recently moved to Kansas City from Pittsburg, Kansas, to work as a personal trainer as part of an internship with the University of Kansas School of Medicine. A client who knew of Corie's fainting episodes recommended she make an appointment with Ashley Simmons, MD, a cardiologist at The University of Kansas Health System.
Dr. Simmons recommended a series of diagnostic tests – including a stress echocardiogram and tilt table test – to determine the cause of Corie's fainting. Both the echocardiogram and chest monitor tests came back normal. Minutes before her tilt table test, however, Corie fainted.
"Her heart actually stopped for 8 seconds," Dr. Simmons recalls.
That day, Corie was diagnosed with autonomic dysfunction, and more specifically, sinus node dysfunction. Sinus node dysfunction, also called sick sinus syndrome, is a condition in which the heart's natural pacemaker does not function properly. This causes the heart to beat either too slowly (as in Corie's case) or too quickly.
Autonomic dysfunction refers to an issue with the autonomic nervous system, which controls automatic body functions like sweating, digestion, heart rhythm and blood pressure.
"The body normally keeps the heart rate and blood pressure the same," says Rhea Pimentel, MD, electrophysiologist at The University of Kansas Health System. "Patients with autonomic dysfunction don't have that same type of control."
According to Pimentel, Corie suffered from a type of autonomic dysfunction called vasovagal syncope. This caused her body to overreact when triggered by certain stressors, like the sharp prick of a needle.
"We didn't even have to complete the tilt test to diagnose her," Dr. Pimentel says. "Once she received an IV, the pain caused her body to respond by drastically dropping her blood pressure and heart rate."
Dr. Simmons and Dr. Pimentel recommended Corie have a pacemaker placed to regulate her heart rhythm. Unlike many traditional pacemakers, however, Corie's includes a novel algorithm and sensor to pace the heart more quickly when a decline in heart rate is detected. This helps reduce the risk of fainting.
"A quarter of people over age 75 need a pacemaker, but in young patients like Corie, it's rare," says Dr. Simmons. "We don't put pacemakers in young women unless they really need it."
On the surface, the 26-year-old personal trainer and competitive weight lifter does not look like a typical pacemaker candidate. But because of the severity and frequency of her fainting spells, and her close call on the freeway, Dr. Simmons and Dr. Pimentel determined that a pacemaker was her best option. Although initially reluctant, Corie agreed to the treatment and had the pacemaker placed within 3 days of her fainting episode.
"It was kind of a shock," Corie recalls. "It's scary to be told you're going to have heart surgery. There are a lot of activities I do. I didn't want this to affect my life."
Corie has not let her diagnosis slow her down. In addition to working 3 jobs, taking a night course and working toward a master's degree, she also trains for and competes in heavy lifting.
"I'm a very busy person," Corie says. "I still work out. I still train. There are certain kinds of lifts that I don't do, and I try to be aware of how I'm feeling."
Corie sees Dr. Simmons every 6 months for checkups to make sure her device is working properly. So far, she has not experienced any recurrent fainting episodes and says she feels more grounded and less lightheaded.
"I didn't realize how bad it was until I didn't feel bad anymore," she says. "Honestly, I was emotional about it [the pacemaker] at first. It's only been a year and I'm still getting used to it. But so far, it's been okay."
Fainting is medically referred to as syncope and involves a temporary loss of consciousness. Syncope usually occurs because of low blood pressure and insufficient oxygen to the brain. It can result from several different factors, including stress, dehydration, rapid changes in blood pressure, heat exhaustion and others. While frequent fainting may not be a sign of an underlying condition, some forms of syncope may suggest a serious disorder.
"Anyone who has recurrent episodes of fainting, or who faints while driving, needs to be evaluated by a cardiologist," says Dr. Simmons.
If you are experiencing syncope, call 913-588-1227 to schedule an appointment with a heart rhythm specialist.

Electrophysiologist Raghu Dendi, MD, heads the autonomic dysfunction clinic at The University of Kansas Health System. Thorough testing is used to determine the underlying causes of syncope and identify the most appropriate treatment. If necessary, patients may receive an evaluation with a neurologist.