- Home
- Types & Treatments
- Proton Therapy
- Proton Therapy FAQ
Frequently Asked Questions About Proton Therapy
Soon, adults and children who have cancer will not be forced to travel out of state to receive lifesaving proton therapy. The innovative and highly precise radiation therapy will be provided through The University of Kansas Cancer Center, the region’s only National Cancer Institute-designated comprehensive cancer center, beginning in spring 2022.
Construction on the proton therapy site began early in 2020. When completed, The University of Kansas Cancer Center’s multimillion-dollar Proton Therapy Center will provide lifesaving treatment for adults and children from throughout the region close to home.
By providing proton therapy here, our cancer patients can remain closer to their home, family and much-needed support systems. The University of Kansas Cancer Center’s Proton Therapy Center will be the first in Kansas and in our region. There are no proton centers in Iowa, Nebraska, Colorado and Arkansas. There are currently 38 proton therapy centers in the United States.
To learn more about the most advanced and precise form of radiation therapy available today, we visited with Ronny Rotondo, MDCM, FRCPC, medical director of proton therapy at the cancer center.
Q. What is proton therapy?
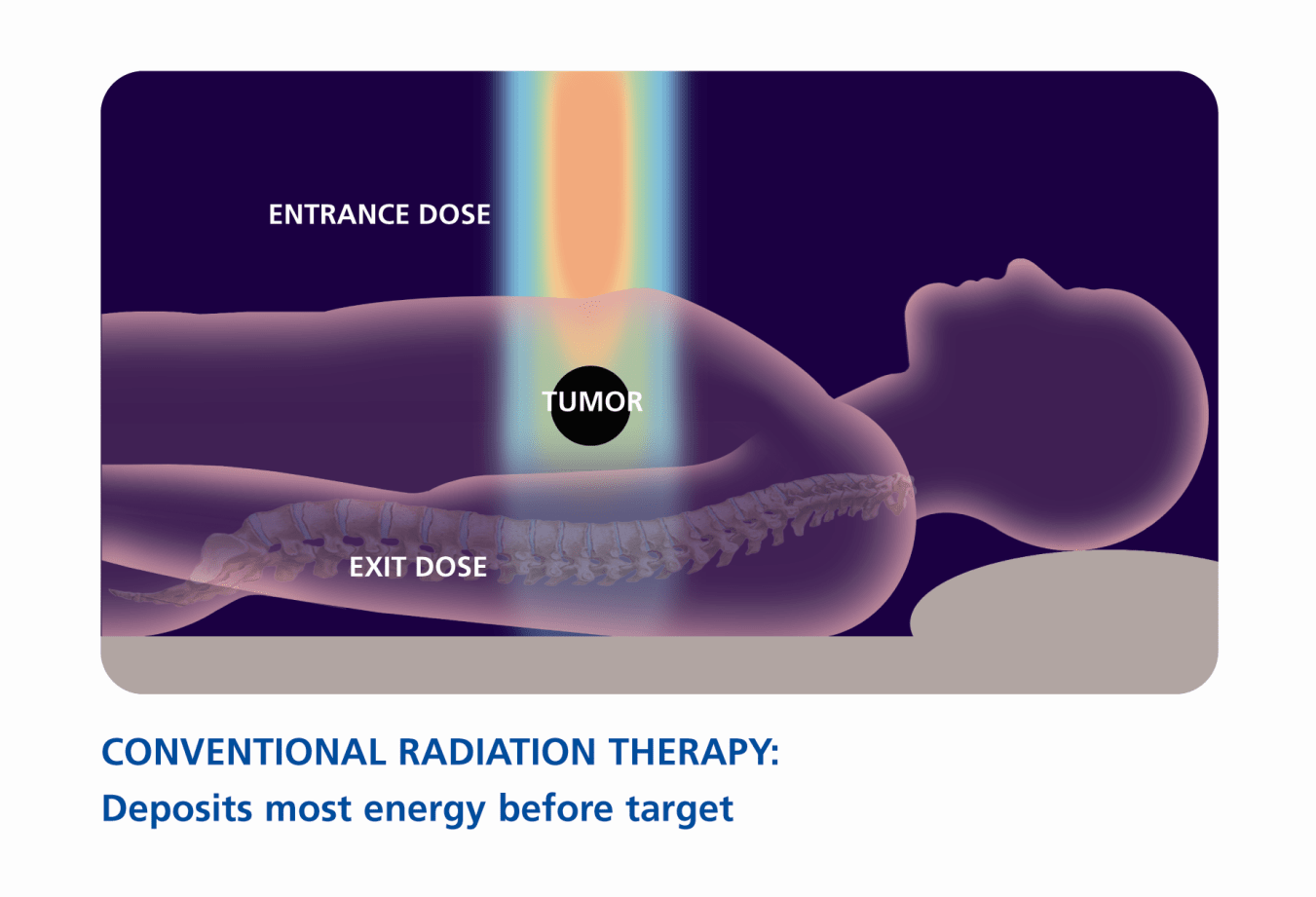
A. Proton therapy is a form of external beam radiation that uses energized protons to deliver radiation to a tumor, whereas conventional radiation uses X-rays or photons. When photons interact with tissue during treatment, they deposit a significant dose of radiation along the entrance path to the tumor, within the tumor target and beyond the tumor as they exit the other side of the body. This results in the delivery of unnecessary radiation to healthy tissues and organs and leaves a trail of potential injury to healthy tissue beyond the tumor target.
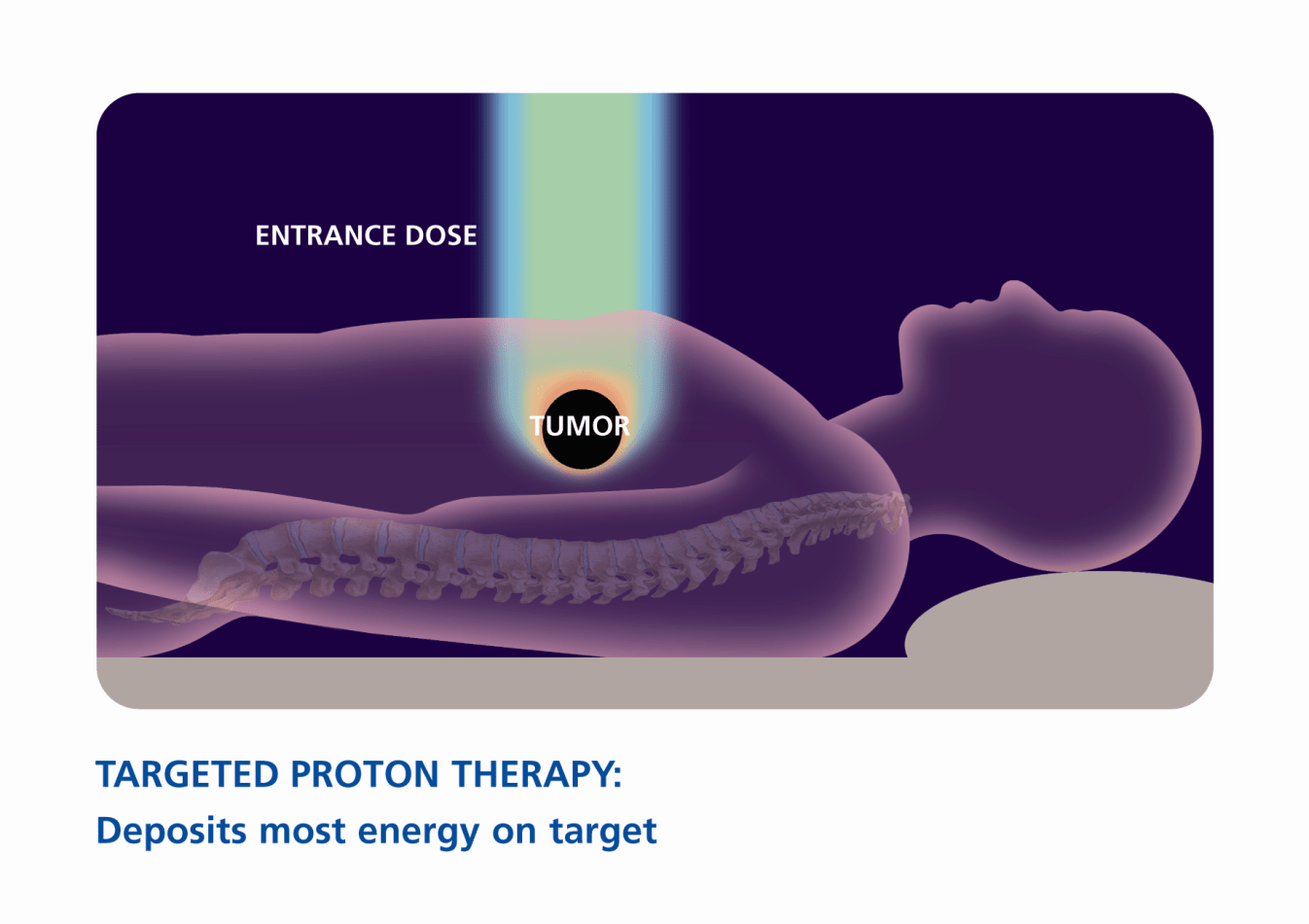
With proton therapy, energized protons interact with healthy tissue differently. There is a lower dose along the entrance path to the tumor and most of the radiation is deposited within the tumor target. Beyond the target, there is no exit dose; radiation does not travel beyond the target. This allows us to target and focus the radiation much more precisely, concentrating radiation in the tumor, where it will benefit the patient, and minimizing radiation to the surrounding healthy tissue. As a result, proton therapy may offer patients the possibility of fewer side effects and improved quality of life, both during and after treatment.
Q. What types of cancer does proton therapy treat?
A. Proton therapy is beneficial for treating most localized solid tumors/recurrent tumors that are close to critical organs/structures because it provides such focused and precise delivery. This includes tumors of the ocular area, brain, skull base, spine, sinonasal and head and neck, and hepatobiliary system (liver, gallbladder, pancreas).
It’s especially beneficial in treating pediatric cancers, as children are particularly sensitive to the effects of radiation and even low doses can have a significant impact on their growth and development. Lower radiation dose to the body also means we may be able to significantly decrease the risk of a secondary radiation-induced tumor. In pediatric patients, proton therapy may be beneficial to treat a wide variety of tumors including tumors of the brain, skull base and spine, chest, abdomen and pelvis, and most tumors that are close to sensitive structures such as the heart or spinal cord.
Overall, a variety of patients can benefit from this type of treatment, and we continue to investigate additional therapeutic opportunities where proton therapy may be appropriate.
Proton therapy may be beneficial for treating cancers of the:
- Bone
- Brain
- Breast
- Central nervous system
- Esophagus
- Eyes
- Head and neck
- Liver
- Lung
- Lymphatic system
- Pancreas
- Pediatric cancers
- Prostate
- Recurrent tumors (reirradition)
Q. How is proton therapy different from photon radiation treatment?
A. Traditional radiation delivers X-rays, or beams of photons, to the tumor and beyond it. This can damage nearby healthy tissues and cause serious side effects. In contrast, proton therapy delivers a beam of proton particles that stops at the tumor, so damage to nearby healthy tissue is minimized.
Proton therapy vs. conventional X-ray
Q. Who is eligible for proton therapy?
A. As was mentioned previously, there are commonly recognized indications for proton therapy. That said, each case must be evaluated separately, with all factors considered. Just because a patient has a type of cancer that can be treated with proton therapy does not mean that patient will benefit from this type of treatment.
We are available and happy to meet with patients to discuss their cancer diagnosis to determine what type of treatment will benefit them most. We encourage anyone who has received a cancer diagnosis to contact us so we can discuss treatment options best suited to their situation. The University of Kansas Cancer Center is the only center in this region that will be able to offer every treatment option available – so that each patient can receive the most appropriate type of radiation treatment, including proton therapy, for their diagnosis.
Q. How can I schedule a consultation for proton therapy?
A. To schedule a consultation for proton therapy, call nurse navigation at 913-588-3671 to learn if proton therapy is a treatment option for you.
Q. Where is the Proton Therapy Center located?
A. The Proton Therapy Center is at:
Richard and Annette Bloch Radiation Oncology Pavilion
4001 Rainbow Blvd.
Kansas City, KS 66160
Q. Why is it important to offer proton therapy at an academic medical center with a National Cancer Institute-designated comprehensive cancer center?
A. NCI-designated comprehensive cancer centers, such as The University of Kansas Cancer Center, are recognized for their scientific leadership in laboratory and clinical research. In addition to serving communities across the state of Kansas and in western Missouri, our impact is broadened because we integrate training and education for biomedical researchers and healthcare professionals.
We dedicate significant resources toward developing research programs, faculty and facilities, such as proton therapy, that will lead to better and innovative approaches to cancer prevention, diagnosis and treatment. Our renowned cancer experts bring vast knowledge and experience to help patients conquer cancer. That expertise also exists in using proton therapy as a tool to help our patients fight cancer.
By bringing this innovative treatment here, we will also have unlimited opportunities to continue research on proton therapy for new and expanded uses in the future. Proton therapy will benefit adult and pediatric patients alike and further advance our research and education missions as one of the nation’s leading cancer centers.
Proton Therapy: A New Tool in Cancer Care
Speaker 1:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
Dr. Roy Jensen:
Myrna Palmer:
Dr. Roy Jensen:
Myrna Palmer:
We were able to get in, have that surgery, and I met Dr. Rotondo the day of my recovery, and he was introducing me to proton beam therapy. It was not available yet in Kansas but I was able to go to the Mayo Clinic in Phoenix and it was a wonderful experience. I just want to tell people that it was... With knowing now what that process is, I wanted just to encourage others with a wonderful experience because it is the... Going over to... I don't know if you want me to go into detail but we were able to go in and have a MRI and CT scan. They formed a mask over my head and pinned me, basically snapped me to a table, but I was told about what this would be and that they gave me so much confidence and just peace that this was going to be a good experience.
I really did try to hear or listen in while that was going on and I have to tell you that it was just an unbelievable thing. At one point, I saw a bright white light come from my right eye and then in another time it was a blue light flash. And other than a little popping in my ear, that was all that I was able to hear or feel during that proton beam experience. They give you some wonderful music to listen to, also your choice. But I just wanted to tell you that the type of cancer that I had was rare and it is... Especially where the location of it was in my brain, but I believe that through this experience, I have to tell you, I trusted the Lord and all of the contacts that were given to me both with the professional doctors, my friends, my family, they were just so supportive and I'll just say that it was just an unbelievable experience. I loved it.
Dr. Roy Jensen:
Myrna Palmer:
Dr. Roy Jensen:
Dr. Ronny Rotondo: Right. So again, proton therapy is a form of external beam radiation therapy. But again, it's a particle therapy as opposed to x-rays or photons. And so, because of the unique characteristics in which it interacts with tissue, again, it focuses the radiation. We're able to concentrate the radiation within the tumor and much more effectively reduce or limit the radiation exposure and the surrounding tissues.
And so, one area where proton therapy can offer significant benefit is in cases like her case with a skull-based Chondrosarcoma where these tumors tend to be relatively radio resistant in the sense that we tend to have to use much higher doses of radiation than we normally would but because of the anatomic location, there's a lot of critical structures in the vicinity including optic chiasm or nerves that are important for vision, cochlea for hearing, the brain and temporal lobe. And so, in such cases and particularly when we're going at high doses near those structures, proton therapy can more effectively concentrate those high doses in the target and spare those critical structures. Decreasing the risks of things like vision loss, hearing loss, and importantly, reducing significantly the dose to the brain which can help decrease the risk of neurocognitive effects so issues with memory, concentration, IQ. All of these things have a significant impact on quality of life.
Dr. Roy Jensen:
Roma:
Dr. Roy Jensen:
Roma:
Dr. Roy Jensen:
Roma:
Dr. Roy Jensen:
Karen Larson:
Dr. Roy Jensen:
Karen Larson:
Dr. Roy Jensen:
Karen Larson: Yeah. Well, proton therapy was just one of five modalities that Roma went through. We started with chemotherapy, then he had an operation to... Chemotherapy to shrink the tumor, an operation to remove the tumor, a stem cell transplant to clear anything residual that might be left in his bones, and then we went to proton therapy, was the first modality, and we finished off with immunotherapy. So proton therapy was four of five modalities that we went through.
Dr. Roy Jensen:
Karen Larson:
Dr. Roy Jensen:
Karen Larson:
Dr. Roy Jensen:
Dr. Roy Jensen:
Roma:
Karen Larson:
Roma:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
Depending on the location of the tumor, the benefits or impact on quality of life may be different. For instance, for a patient with a brain tumor it might be less hair loss, less fatigue, less nausea. For head and neck cancer patients, there's data showing that there's less pain associated with radiation for swallowing, less need for feeding tubes. For abdominal tumors or for instance, like Roma's, radiation significantly decreases exposure to the gastrointestinal systems so bowel and stomach and so forth. And so, that can significantly decrease, again, impact on nausea or bowel movements.
Overall, I would say that patients tolerate treatment quite well. Many of them are able to continue to go to school, continue to go to work, and live normal lives. And that in many instances, proton therapy, again, not only can improve quality of life with long term effects, but in many instances, also during treatment, patients seem to do better.
Dr. Roy Jensen:
If you're joining us, we're here with Dr. Ronny Rotondo and Myrna Palmer, a nurse in cancer patient who has undergone proton therapy, along with Karen Larson and her son Roma who underwent proton therapy. We are discussing proton therapy as an exciting new tool to treat cancer. Remember to share this link with people you think might benefit from our discussion. Use the hashtag #BenchToBedside. So Dr. Rotondo, exactly when will the new proton center at KU be open?
Dr. Ronny Rotondo:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
So one can imagine, for instance, a tumor that arose in proximity to the spine or the spinal cord and they've received prior radiation. With conventional radiation, it may not be feasible to re-treat because of already having received maximum dose of the spinal cord. Proton therapy may be able to overcome that hurdle. And so, it's certainly an area where there's a lot of research and very good consideration. So certainly, patients with recurrent cancer that would be good inquiry.
Dr. Roy Jensen:
Myrna Palmer:
Dr. Roy Jensen:
Roma:
Dr. Roy Jensen:
Myrna Palmer:
Dr. Roy Jensen:
Karen Larson:
Dr. Roy Jensen:
Dr. Ronny Rotondo:
In addition, we will have clinical trials open with other national groups like the NRG or also collaborations with other institutions across the country for clinical trials which involve proton therapy, whether they're direct comparisons with photon therapy or trials that allow or include proton therapy. As part of our program, we've also included the capability to perform cellular and kind of small and large animal research. And so, we have the facilities and resources to be able to conduct those studies and those plans are actually currently underway.
Part of our research program will also include very active research program in the medical physics component of proton therapy including things like flash therapy. And so, we'll be collaborating with IBA to lead some studies in flash therapy as well. And so, very excited about our research program.
Dr. Roy Jensen:
Dr. Ronny Rotondo:
I think there will continue to be improvements in terms of image guidance, treatment delivery techniques, flash therapy, which is a term that people will increasingly hear of but it's a very exciting area of research where we may potentially be able to deliver entire courses of radiation in a single treatment or several treatments as opposed to many weeks. We're not quite there yet but I think there's some very exciting developments in the future for proton therapy.
Dr. Roy Jensen:
Dr. Ronny Rotondo:
Dr. Roy Jensen:
Karen Larson:
I mean, I think the final thing to say about Roma and proton beam therapy is that he continues to grow at an average rate. He continues to... He's doing great in school. Most people would never have any idea at all, just by what he looks like today and his performance in school and he's active in sports, that he had gone through such a traumatic experience as a child.
I remember when we were initially consulted about radiation, typical radiation, not proton beam, they gave me a list of side effects that would happen after typical radiation. It was one of the most depressing conversations, I think, we'd had during his whole treatment. But the doctor said, at the time, if you can get proton beam therapy, that significantly lowers your risk of these side effects.
Now, of course they can't guarantee 100%, but it significantly lowers those risks. And so, for us that was a... We were lucky enough to travel for it, that was a no-brainer what to do. I guess in closing, I think Roma is a pretty good testament to how successful proton beam radiation can be as well as other medical development because he had a really tough diagnosis but he continues to thrive and has been in remission for six years now. So, very exciting.
Dr. Roy Jensen:
Roma:
Karen Larson:
Roma:
Dr. Roy Jensen:
Myrna Palmer:
And so, I would encourage others to look forward also for all the benefits that go with going through an experience with others and sharing with others. I think, in the waiting room, I was talking to other patients and just early on and later we were all helping each other just through this process and it was so interesting to hear how people were just very surprised at how comfortable the whole experience was and the wonderful benefits that we all got. I have a clear MRI and CT scan and someone would say it is inactive, but I claim no longer active. This is dead to me. And so, I go forward healed and it's because of proton beam therapy. I think-
Dr. Roy Jensen:
Myrna Palmer:
Dr. Roy Jensen:
Myrna Palmer:
Dr. Roy Jensen: