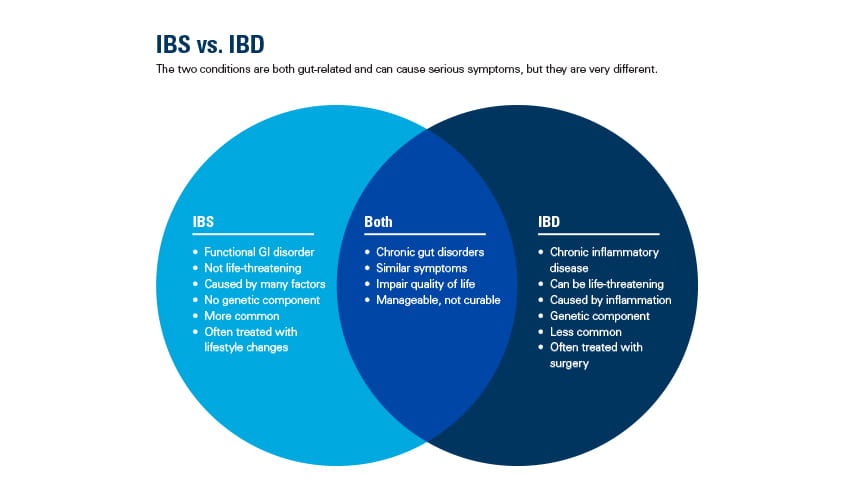
People often confuse irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Both are common illnesses that affect the gut, have similar symptoms and affect a person's quality of life. But IBS and IBD are very different, despite their almost identical acronyms. The disease process, the damage it can wreak on your body and the long-term outcomes can vary greatly. In fact, one can be life-threatening if it isn't treated early.
Understanding the differences between IBD and IBS is important for an accurate diagnosis and effective treatment plan. If you think you might have one or both (yes, they can occur together) of these conditions, here's what you need to know.
Understanding IBS
IBS is the most common disease diagnosed by gastroenterologists. It's also one of the most common disorders seen by primary care physicians, according to the American College of Gastroenterology.
IBS is a disorder of how the gastrointestinal (GI) tract works. It can take many forms, including IBS-C (causing constipation), IBS-D (causing diarrhea) or IBS-M (a mix of constipation and diarrhea). IBS is difficult to detect, which can be frustrating for individuals who struggle with the discomfort of daily symptoms.
Diarrhea can result when the GI tract moves too fast, and constipation may result when it moves too slowly.
In addition to diarrhea and constipation, other signs that suggest IBS include:
- Abdominal pain, bloating, gas
- Normal appearance of colon
- Normal lab tests with no inflammatory markers
- A family history of IBS
Diagnosing and treating IBS
Blood tests and a thorough understanding of your medical history and symptoms are the most common ways IBS is diagnosed. Still, physicians aren't sure what causes it. But they do know stress and certain foods can trigger flare-ups. To manage symptoms, try this 3-step plan:
- Change your diet. Eliminate gluten and dairy and eat a low-FODMAP diet (foods that cause gas, bloating and possibly diarrhea).
- Add fiber. Take a fiber powder supplement and drink plenty of water.
- Reduce stress. Eliminate the stress you can. Learn to better manage the stress you can't. Meditation and regular exercise can help ease symptoms.
There are other medical options for IBS, such as an FDA-approved antibiotic that helps those with IBS-D. For those with IBS-C, some antidepressants can help, too.
If diarrhea persists longer than 6 weeks despite managing stress and improving diets, see a primary care physician.