Rapid Action Is First Step in Saving Arm


February 22, 2019
Steve Pelegrin built a 20-year career as an engineer with a major telecommunications company and enjoys a good home improvement project. In February 2015, he was a newlywed, just several months into his marriage to his wife, Laurie. Working alone on a basement remodeling project, an accident occurred that put his ability to function, and his life, at risk.
Nearly finished cutting some small pieces of wood, Steve stood, turned and snagged his shirt in the blade guard of an electric saw. The saw caught and almost completely severed Steve's left arm.
Steve's survival training – he was once a U.S. Army Ranger – and ability to remain calm saved his life and preserved the potential to restore his limb. Steve used his right hand and his teeth to remove his belt and apply it as a tourniquet to stem the bleeding at his left forearm. He climbed the stairs from the basement and called 911. He put the couple's dogs in the backyard and went out to sit on the front curb and wait for help.
"Steve truly had the presence of mind to save his own life that day," says Laurie, who works as a surgical assistant at their local hospital in Ottawa, Kansas. "He could have bled out alone in the basement. His training and instinct to survive gave him a chance."
When the ambulance arrived, the emergency response team began asking questions to learn about Steve's injury and history.
"I remember telling them, I'll answer whatever you want on the way, but we better get going now,'" Steve says. "I can't say enough good things about the quality of care and the experience they provide. If we hadn't had access to this caliber of care, I would have had a very different result, for sure."
The response team knew that Steve needed more advanced care than the local hospital could provide. Steve was taken to a nearby Level II Trauma Center, but that wasn't enough. The care team there immediately transferred Steve to The University of Kansas Health System, which offers the region's most experienced Level I Trauma Center verified by the American College of Surgeons. Only here would Steve find the specialty-trained plastic and reconstructive surgery specialists he needed for the best chance at successful replantation.
"There were a lot of people in white coats ready and waiting for me when the ambulance arrived," Steve recalls. "We were so fortunate to have a Level I Trauma Center so close to home."
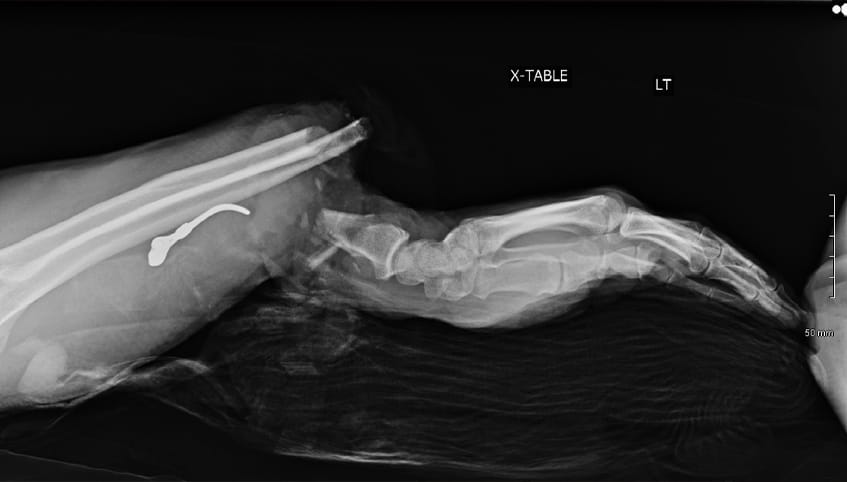
A surgical team performed an intricate 8-hour microsurgery to reattach Steve's forearm. Having completed fellowships in hand and upper extremity surgery, and addressing traumatic injuries such as this on a weekly basis, the team offered some of the region's best care in replantation and functional recovery.
Surgeons performed Steve's surgery under a microscope. They first plated and screwed the severed bones into place and then used sutures finer than a human hair to reconnect transected nerves, veins, blood vessels and tendons.

The care team is able to begin care even before the patient arrives, which is essential since the separated body part is viable for only about 4 hours. They collaborate with the referring providers to start antibiotics, transfer X-rays or instruct the use of splints. By getting started immediately, the team can make the most of limited time.
The surgeons also performed a fasciotomy, in which the closed compartments that contain the hand muscles are opened to allow room for muscle expansion. Muscle inflammation is common, and if this occurs without space to expand, the tissue swells and may die.
After the surgery, Steve began what he considered the most challenging part of the journey.
"For 24 to 48 hours after the surgery, we didn't know if the limb was going to take," Steve says. "The waiting was the hardest part."
Steve spent 9 days in the hospital's "tropicana room," in which the temperature is kept above 80 degrees to promote blood flow to the extremities. During this period, Steve's care team examined the arm frequently to assess for arterial or venous insufficiency – problems with the blood moving into or out of the limb. If such problems are found, surgical adjustments can be made, but none were needed in Steve's case.
Steve then began rehabilitation therapy while still in the hospital.
"With traumatic injuries such as this, it is important to limit active range of motion immediately following surgery," says Janelle Epp, Steve's inpatient physical therapist. "Active range of motion exercises can cause the tendons to separate at the repair site. Passive range of motion exercises were performed to keep the joints moving and provide tendon glide to prevent adhesions."
Before discharge, Epp prepared 2 splints for Steve, 1 to allow motion at the elbow while preventing forearm rotation, and the other to prevent flexion contractures – the curling in of the fingers – during sleep. She taught Laurie to apply the splints and to help Steve with his exercises.
Steve continued therapy with a certified hand therapist located close to his home. With hard work that Laurie said "made him sweat," he was back on the job in 8 months.
The team there is absolutely wonderful. I can't say enough good things about the quality of care and the experience they provide. If we hadn't had access to this caliber of care, I would have had a very different result, for sure. – Steve Pelegrin
Today, Steve considers his left limb a "helper," beneficial in supporting his dominant right hand in accomplishing daily tasks. The replanted limb has limited dexterity, but can hold things and feel hot and cold. It is useful in routing circuits on the job, though tasks take more time than they once did.
"I used to be able to do anything and everything I wanted, and now I have issues and limits," Steve says. "That is a frustration and strange to get used to. It is challenging to have to work a little slower, but at least I am able to work. I am truly thankful for what I've got."
Steve credited The University of Kansas Health System for his positive outcome.
"The team there is absolutely wonderful," he says. "I can't say enough good things about the quality of care and the experience they provide. If we hadn't had access to this caliber of care, I would have had a very different result, for sure."
Steve's care team says that getting to the OR quickly was critically important to successfully reestablishing blood flow. He also benefited from focusing on rehabilitation therapy. With all the care team's skill and experience in replantation, Steve's good outcome depended on his commitment and hard work, which he gave.
Laurie is thankful for the strength of Steve and his care team.
"People tend toward fight or flight," she says. "Steve fought. He stayed calm and kept his head. We are very, very lucky for that, and lucky to have The University of Kansas Health System so close to home."